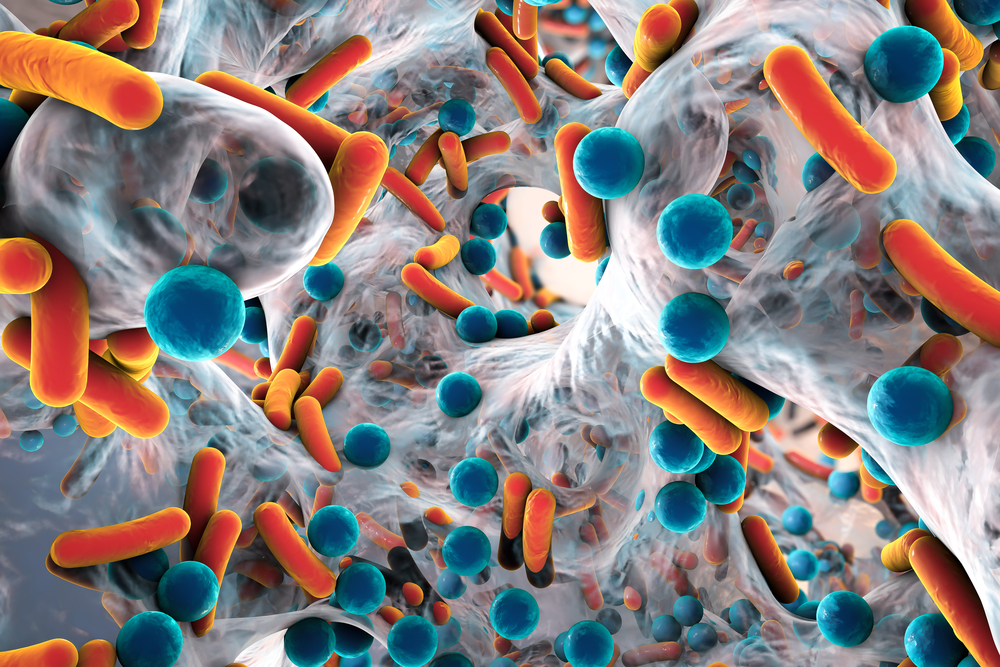
Humanity has fallen behind in the fight against drug-resistant bacteria, but AI could prove to be our secret weapon.
Antibiotic-resistant pathogens are responsible for between 1 and 5 million deaths per year.
Few new antibiotics have been developed over the last decade, and the majority are slight tweaks to existing antibiotics.
Discovering new drugs is exceptionally labor-intensive, but a recent landmark study has harnessed AI to automatically screen thousands of compounds to uncover avenues for lab testing.
The study, published in Nature Chemical Biology, saw researchers from MIT and McMaster University attempt to discover new drugs to kill Acinetobacter baumannii, a bacteria the WHO identified as a “critical threat.”
Researchers used two machine learning (ML) models to automate the drug discovery process in silico, which means “in a computer.”
Here’s how it worked:
Obtained training data
- The researchers exposed lab-grown A. baumannii to about 7,500 different chemical compounds and monitored to see which compounds inhibited the growth of the microbe.
- The chemical structures of those that inhibited growth were fed into a machine learning (ML) model. This enabled the model to learn the chemical features associated with growth inhibition.
Trained and tested the model
- Once the model was trained, the researchers used it to analyze a set of 6,680 compounds that the model had not previously encountered. These compounds were sourced from the Drug Repurposing Hub at the Broad Institute. It singled out a few hundred compounds.
- The researchers chose 240 from the shortlist to test experimentally in the lab.
- They focused on compounds with differentiated structures to existing antibiotics, as this makes them more likely to evade antibiotic resistance.
Experimental lab testing
- Lab tests narrowed the list to 9 antibiotics.
- Among these, one compound initially explored as a potential diabetes drug was found to be extremely effective at killing A. baumannii. The drug was called “abaucin”.
- Peculiarly, it did not affect other species of bacteria, including Pseudomonas aeruginosa, Staphylococcus aureus, and Enterobacteriaceae.
Dr. Stokes, who worked on the project, told the BBC, “This is when the work starts.”
The antibiotic will undergo a lengthy testing procedure to gauge its safety in humans, which may not be complete until 2030.
Even so, AI accelerates the labor-intensive task of exploring new drugs, helping researchers uncover interesting and novel antimicrobial compounds. Many have been developed for other purposes, so they’re already out there – we just need to find them.
Dr. Stokes said, “AI enhances the rate, and in a perfect world decreases the cost, with which we can discover these new classes of antibiotic that we desperately need.”
While testing safety in humans remains a slow process, AI-supported research pipelines are sure to accelerate time-to-market for antibiotics and other pharmaceuticals.